Everyone knows that when you’re pregnant, you’re eating for two. Less obvious, however, is knowing the particular foods pregnant women shouldn’t eat in order to avoid infectious, food-borne diseases, as these can cause miscarriage, low birth weight or a higher risk of Mum getting sick.
Know your infectious diseases
The several food-borne infections that are particularly dangerous during pregnancy are:
Bad news: Listeria monocytogenes infection (listeriosis)
Listeriosis is relatively uncommon, but if contracted, it can be incredibly bad news. This bacteria, found in raw meat and soft cheeses, causes respiratory problems, brain inflammation and blood infection. For the baby in the belly, it can unfortunately lead to miscarriage, stillbirth, premature birth or pneumonia when they are born.
Cat poos: Toxoplasma gondii infection (toxoplasmosis)
Toxoplasma gondii is an organism found in raw meat and cat faeces. A Mum can transport the organism to the bub in the womb. While it doesn’t usually lead to miscarriage, toxoplasmosis is associated with very negative effects, such as:
- Eye inflammation;
- Mental retardation;
- Hearing loss;
- Blindness; and
- Epilepsy.
In the raw: Salmonella infection (salmonellosis)
Salmonellosis is an infectious disease caused by the bacteria Salmonella. It is found in raw animal products (including eggs) and some plant foods (in particular sprouts). It causes nausea, vomiting, abdominal cramps, diarrhoea, fever and headache. While pregnant women are no more likely than those in the general population to experience salmonella infection, it has been linked to miscarriage, and therefore the consequences of infection are more serious for pregnant women.
Keeping nasties at bay
Preparing and storing food hygienically, or avoiding some foods, is the best way to keep the nasties at bay.
Hygiene measures
Maintaining good personal hygiene during pregnancy can reduce the risk of food-borne illness, and particularly illness associated with toxoplasmosis from infection with the bacteria T. gondii. This infection often occurs as a result of contamination from unwashed hands which have been in contact with animal faeces, rather than from contaminated food.
Hygiene measures pregnant women should take to avoid the risk of toxoplasmosis and other infectious diseases include:
- Wash hands thoroughly before preparing or eating food and after gardening or touching pets;
- Avoid cat litter, including changing the kitty litter tray; and
- Wear gloves when gardening.
Food preparation measures
Women who are pregnant or trying to conceive should take additional hygiene precautions when preparing food to reduce the risk of infection. These include:
- Ensure benches, utensils and other food preparation equipment is clean, particularly if it has previously been in contact with raw meat or vegetables;
- Avoid raw meat contaminating other foods by using separate utensils (especially knives and cutting boards) for raw meat and other foods, and keeping them in a separate section of the refrigerator;
- Always eat well-cooked meat. Meat is thoroughly cooked when no pink sections are visible (even in the centre of the meat portion) and the juices run clear;
- Thaw frozen food in the refrigerator or microwave. Food should not be left on a bench or in the sink to defrost;
- Reheat food to steaming hot (> 60°C) and ensure leftover food is kept cold (< 5°C) until it is ready to be reheated and eaten; and
- Wash raw foods before eating and wash hands after handling raw foods.
Food to avoid
Pregnant women can reduce their chance of food-borne illnesses during pregnancy by avoiding some types of food. In general it is recommended that pregnant women only eat freshly prepared foods. Leftovers from home-cooked meals can be eaten within 24 hours if they are properly refrigerated at < 5°C. However, takeaway foods may spend considerable periods of time in warming ovens or displays and should be avoided.
Pregnant women should also avoid the following foods:
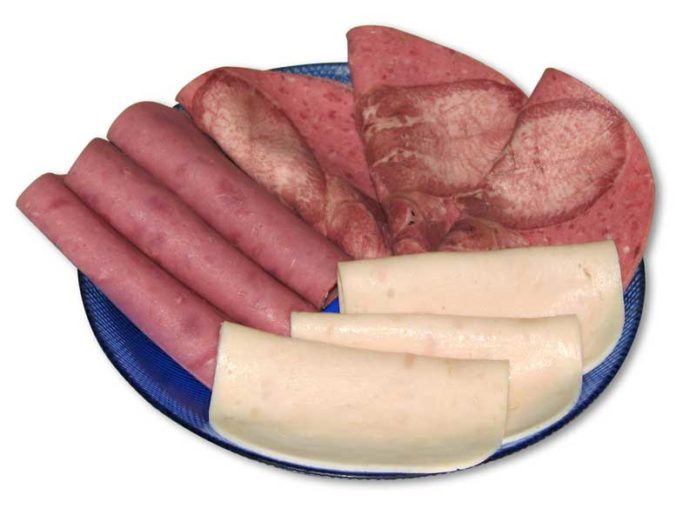
- Raw meat, including raw seafood and raw eggs;
- Unpasteurised milk and other dairy products;
- Soft-serve icecream;
- Soft cheese and patés;
- Chilled ready-to-eat foods, including;
- Cold cooked chicken;
- Processed meats;
- Prepared salads;
- Ready-cooked takeaway foods;
- Leftovers tht are more than 24 hours old or that have not been refrigerated at < 5°C;
- All types of sprouts, including alfalfa, broccoli, onion, sunflower, clover, radish and snow pea sprouts; and
- Mung and soy beans.
Toxic avengers
As well as carrying the risk of infections, some foods may also be toxic (poisonous) if consumed in large quantities by pregnant women … and since a new Mum is eating for two, look out for these particular elements.
Mercury rising
Excessive mercury consumption during pregnancy may cause toxicity, which can harm the developing foetus. Mercury occurs naturally in the environment and is also a component of industrial pollution, so it can often end up in the fish we eat.
To avoid mercury toxicity, pregnant women should limit their consumption of fish, as all types of fish contain traces of mercury. The NSW Food Authority recommends that women eat no more than:
- 2–3 serves of fish per week, where 1 serve is 150 g of fish;
- 1 serve of shark (flake) or billfish (Broadbill, Swordfish or Marlin) per fortnight. Women who consume shark or billfish should not consume any other servings of fish in the fortnight;
- 1 serve of orange roughy (sea perch) or catfish per week. Women who consume a serving of orange roughy or catfish should not consume any other servings of fish in the week.
Products like seafood sticks usually have low levels of mercury, so 2–3 serves of these products each week is safe.
Importantly, mercury actually builds up in the body over time. So ladies planning a pregnancy should also limit their fish consumption, as it takes several months for mercury levels in the body to decrease.
Caffeine
High levels of caffeine intake (> 300 mg/day) during pregnancy are potentially harmful. Evidence suggests that consuming > 300 mg of caffeine per day during pregnancy increases the risk of intrauterine growth retardation (restricted growth in the womb) and spontaneous abortion. It is not yet known whether consuming smaller quantities of caffeine presents health risks during pregnancy.
Ideally, it is best for bub to eliminate caffeine altogether, but if you need a fix, make sure you don’t consume more than the following daily limits;
- 1 mug of ground coffee;
- 2 mugs of instant coffee;
- 2 mugs of tea;
- 5 cans (1.8 L) of cola drink;
- 2 cans (500 mL) of energy drink;
- 4 (50 g) bars of plain chocolate; or
- 8 (50 g) bars of milk chocolate (contains half the caffeine of plain chocolate).
Alcohol
There is strong evidence that high levels of alcohol consumption during pregnancy cause foetal damage and intrauterine growth retardation. It is recommended that pregnant women do not drink at all during pregnancy. If they do drink, it should not be to the point of intoxication.
If you are unsure about a particular food or drink, it’s not worth taking a risk. So speak to your GP or health professional before consumption. If you can’t, then avoid suspicious foods until you are sure both you and your baby are not at risk.



 (7 votes, average: 4.43 out of 5)
(7 votes, average: 4.43 out of 5)